|
|
Developmental Biology - Glioblastoma Brain Cancer
Diabetes Drug Slows Glioma Brain Cancer
Research shows new use of insulin drug could block glioma tumor spread...
A research team from the University of Georgia (UGA) Regenerative Bioscience Center has found that a compound molecule used for drug delivery of insulin could be used to treat glioblastoma, an aggressive, usually fatal form of brain cancer.
Glioblastoma, also known as GBM, is a fast-growing, web-like tumor that arises from supportive tissue around the brain and resists surgical treatment. Described by some as looking for "sand in grass," GBM cells are hard to remove and tend to reach out with tentacle-like extensions throughout the surrounding healthy brain tissue. According to the National Foundation for Cancer Research, more than half of newly diagnosed GBM patients die within the first 15 months of diagnosis. U.S. Senators John McCain and Ted Kennedy both died from GBM, raising national awareness of the deadly disease.
Surfen, a molecular compound first described in 1938, is a pharmaceutical agent used to optimize insulin delivery. UGA researchers have now identified that surfen-treated cells "blocked" the spread and growth of glioma tumor cells in mice brains.
"This study shows that we can stifle the growth of invasive brain tumors with a compound that has a substantial clinical advantage, and can aid in the reduction or refinement of mainstream treatments, particularly radiation and/or chemo."
Lohitash Karumbaiah PhD, Associate Professor, Regenerative Medicine, Regenerative Bioscience Center, University of Georgia, Athens, Georgia, USA.
Published ahead of print in the FASEB Journal, the study is the first known use of surfen as an application to treat GBM.
The research team first used cultured cells to observe the binding properties of the surfen compound. Next, they injected live rodents with cells that could grow into invasive tumors. They then observed how surfen-treated animals had smaller tumors and substantially reduced brain hemorrhage volume than control animals.
"In basic terms, surfen has a high positive charge and binds to negatively charged things. As we study sugars in the brain, which are negatively charged, we asked, 'Why not try using positive charges to block negative ones?'"
Meghan Logun, graduate student working with Karumbaiah, Regenerative Bioscience Center, University of Georgia, Athens, Georgia, USA.
Logun studies how brain cancer takes advantage of highly charged elements in brain tissue to aid its invasion. "In surfen-treated animals, we saw that tumors were actually much more constrained and had more defined boundaries," she explains.
The team worked with Leidong Mao, associate professor in UGA's College of Engineering and co-developer of a microfluidic device that can identify glycosaminoglycans (GAGs) — the highly negative charged molecules produced by brain tumors. Designed to mimic neural pathways of the brain, the device allows real-time monitoring of tumor cell adhesion and thus growth.
"We did not expect to see such a robust response. Blocking off the charged GAGs from the tumor cells really dampened their ability to invade."
Leidong Mao PhD, Associate Professor, University of Georgia, College of Engineering
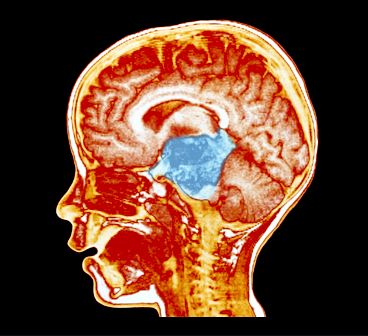
Based on the study's discovery that surfen had isolated the tumor, the team also analyzed MRI images to gauge the treatment's effectiveness.
"In the MRI image you can see [the effects of the surfen treatment] pretty drastically, not in terms of killing the GBM but in blocking its prey," said Qun Zhao, associate professor of physics in the UGA Franklin College of Arts and Sciences and another RBC collaborator on the project. "In the non-treated image, you see rampant invasive growth, compared to the surfen-models where you see a nicely contained and almost circular-shaped tumor."
"The tumor may still grow, but at least now it doesn't have any invasive inroads to creep into other parts of the brain. That could be clinically beneficial for a surgeon wanting to remove the tumor and not having to worry about rogue cancer cells."
Lohitash Karumbaiah PhD.
Looking ahead, Karumbaiah is hopeful that repurposing a compound known to be safe, with proven and beneficial binding properties, could help accelerate review and approval of this potential new therapeutic, and advance consideration in helping to expedite the drug approval process.
"Our hope is that, in the wake of this discovery, lives can be saved, and we can finally change the scope of this life-threatening disease," declares Karumbaiah. "In my five years at UGA, this is the highest profile cancer paper I've ever had."
Abstract
Invasive spread of glioblastoma (GBM) is linked to changes in chondroitin sulfate (CS) proteoglycan (CSPG)–associated sulfated glycosaminoglycans (GAGs) that are selectively up-regulated in the tumor microenvironment (TME). We hypothesized that inhibiting CS-GAG signaling in the TME would stem GBM invasion. Rat F98 GBM cells demonstrated enhanced preferential cell invasion into oversulfated 3-dimensional composite of CS-A and CS-E [4- and 4,6-sulfated CS-GAG (COMP)] matrices compared with monosulfated (4-sulfated) and unsulfated hyaluronic acid matrices in microfluidics-based choice assays, which is likely influenced by differential GAG receptor binding specificities. Both F98 and human patient–derived glioma stem cells (GSCs) demonstrated a high degree of colocalization of the GSC marker CD133 and CSPGs. The small molecule sulfated GAG antagonist bis-2-methyl-4-amino-quinolyl-6-carbamide (surfen) reduced invasion and focal adhesions in F98 cells encapsulated in COMP matrices and blocked CD133 and antichondroitin sulfate antibody (CS-56) detection of respective antigens in F98 cells and human GSCs. Surfen-treated F98 cells down-regulated CSPG-binding receptor transcripts and protein, as well as total and activated ERK and protein kinase B. Lastly, rats induced with frontal lobe tumors and treated with a single intratumoral dose of surfen demonstrated reduced tumor burden and spread compared with untreated controls. These results present a first demonstration of surfen as an inhibitor of sulfated GAG signaling to stem GBM invasion.—Logun, M. T., Wynens, K. E., Simchick, G., Zhao, W., Mao, L., Zhao, Q., Mukherjee, S., Brat, D. J., Karumbaiah, L. Surfen-mediated blockade of extratumoral chondroitin sulfate glycosaminoglycans inhibits glioblastoma invasion.
Authors
Meghan T. Logun, Kallie E. Wynens, Gregory Simchick, Wujun Zhao, Leidong Mao, Qun Zhao, Subhas Mukherjee, Daniel J. Brat, and Lohitash Karumbaiah.
Acknowledgements
This study was funded by the National Institutes of Health and UGA's Clinical and Translational Research Unit. The Regenerative Bioscience Center is a unit of the UGA Office of Research, with generous support from the College of Agriculture and Environmental Sciences and its Department of Animal and Dairy Science.
The authors declare no competing interests.
Return to top of page.
| |
|
Sep 11 2019 Fetal Timeline Maternal Timeline News
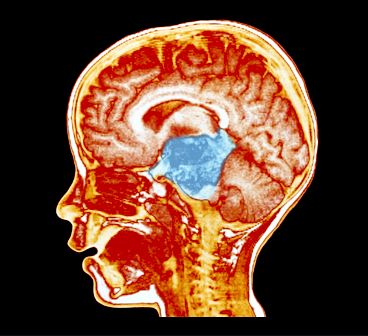 Brain scan, child with glioma. CREDIT Medscape.
|