|
|
Developmental Biology - Circadian Clocks & Diabetes
Could Resetting Circadian Clocks Control Diabetes?
Research demonstrates a link between disturbance in circadian clocks in pancreatic cells - with type 2 diabetes, and can correct that disturbance...
The circadian clock system (Latin "circa diem" meaning: about a day) allows an organism to anticipate periodic changes in physical time, and to adjust to these changes. Nearly all cells in our body have molecular clocks that regulate and synchronize metabolic functions according to a 24-hour cycle of day to night.
Increasing evidence reveals disturbances from frequent time zone changes, irregular working schedules, as well as ageing, have a significant impact on the development of metabolic diseases in human beings, including type-2 diabetes.
Such disturbances seem to prevent proper functioning of pancreatic islet cells which secrete insulin and glucagon, hormones regulating blood sugar levels.
By comparing human pancreatic cells from type 2 diabetic donors to those of non-diabetic donors, researchers at the University of Geneva (UNIGE) and the University Hospitals of Geneva (HUG) in Switzerland, for the first time demonstrated that pancreatic islet cells from Type 2 Diabetic donors have compromised circadian oscillators.
Disruption of their circadian clocks was happening at the same time as perturbations in their hormone secretions. Using a clock modulator molecule called Nobiletin (extracted from lemon peel) researchers succeeded in "repairing" the disrupted cellular clocks and partially restoring islet cell function.
These results are published in the Proceedings of the National Academy of Sciences of the United States (PNAS), and provide our first insight into an innovative approach for diabetes care.
Two years ago, the team at the Diabetes Centre UNIGE Faculty of Medicine and at HUG, led by Charna Dibner, Principle Investigator in the Departments of Medicine and of Cell Physiology and Metabolism, showed that perturbation of pancreatic cellular clocks in rodents led to disruption of their insulin and glucagon secretions, promoting the onset of diabetes. But was the situation in human beings the same?
"We had previously observed that if the clocks of human pancreatic cells were artificially disrupted in cell cultures in vitro, secretion of key islet hormones - insulin and glucagon - was compromised. Our next step was to unravel whether circadian rhythms were perturbed in human pancreatic islets in type 2 diabetes, and if so, how would this perturbation affect islet function."
Volodymyr Petrenko PhD, Division of Endocrinology, Diabetes, and Nutrition, Department of Medicine; Department of Cell Physiology and Metabolism, Faculty of Medicine; Diabetes Center, Faculty of Medicine; Institute of Genetics and Genomics, University of Geneva, Geneva, Switzerland; and first author on the work.
Using combined bioluminescence-fluorescence time-lapse microscopy — a technology that allows very precise tracking of molecular clock activity in living cells over time — scientists were able to compare the behaviour of pancreatic cell of type-2 diabetic donors and non-diabetic subjects throughout the day.
"The verdict is indisputable," says Charna Dibner. The biological rhythms of the islet cells in type-2 diabetes exhibit both reduced amplitudes of circadian oscillations and poor synchronization capacity. "As a result, hormone secretion is no longer coordinated. Moreover, the defects in temporal coordination of insulin and glucagon secretion observed in patients with type-2 diabetes were comparable to those measured in healthy islet cells with artificially-disrupted circadian clock."
It's All In The Timing!
Circadian clocks represent the daily cycles governing our various cellular functions. There are several interlocking levels of synchronization of these clocks, the main one being light which in particular regulates our central clock located in the cerebral hypothalamus.
Like a conductor in an orchestra, the hypothalamus regulates peripheral clocks present in our organs and cells. Cellular clocks are somewhat centrally regulated, yet function differently for each organ; even in each cell, depending on that organ's function.
"Pancreatic cells are also subject to the rhythm of fasting and food intake, and to a tight hormonal regulation. Coordinating all levels of regulation therefore allows for optimized metabolic function. Clocks deregulated in pancreatic islet cells leads to a compromised function: they no longer anticipate food-derived signals."
"Indeed, if you eat the same food, but at night rather than during the day, you may gain weight much faster. This is due to a suboptimal response by your overall metabolism."
Charna Dibner PhD, Division of Endocrinology, Diabetes, and Nutrition, Department of Medicine; Department of Cell Physiology and Metabolism, Faculty of Medicine; Diabetes Center, Faculty of Medicine; Institute of Genetics and Genomics in Geneva, University of Geneva, Switzerland
Setting The Right Time Again
In step two of their research, Geneva scientists used Nobiletin, a small clock modulator molecule - a natural ingredient of lemon peel whose impact on circadian clocks has been recently discovered - in order to resynchronize the metabolic clocks.
"Acting on one of the core-clock components, Nobiletin efficiently resets the amplitude of oscillations in human islets. As soon as we got the clocks back in sync, we also observed an improvement in insulin secretion."
Volodymyr Petrenko PhD.
According to Charna Dibner: "This is the first proof of principle that repairing compromised circadian clocks may help improving the function of the pancreatic islet hormone secretion. We will continue by exploring this repair mechanism in vivo, first in animal models. Our society experiences epidemic growth in metabolic diseases, concomitant with shifted working and eating schedules, and lack of sleep. By re-synchronizing the perturbed molecular clocks, either by personalized eating and exercise schedules or with the help of clock modulator molecules, we hope to ultimately be able to provide an innovative solution to an epidemical metabolic problem affecting an ever-increasing proportion of the world's population."
Significance
Here we report that intact islets and islet cells from type 2 diabetes (T2D) donors exhibit attenuated molecular oscillators bearing lower circadian amplitude and compromised synchronization capacity in vitro. Furthermore, we reveal that secretion profiles of insulin, proinsulin, and glucagon were circadian rhythmic under physiological conditions. The temporal coordination of the islet hormone secretion was perturbed in human T2D islets, concomitant with the islet molecular clock alterations. Strikingly, clock-deficient human islet cells exhibited disrupted insulin and glucagon granule docking and exocytosis. Treating the T2D islets with the clock modulator Nobiletin boosted circadian amplitude and insulin secretion. Our study uncovers a link between human molecular clockwork and T2D, thus considering clock modulators as putative pharmacological intervention to combat this disorder.
Abstract
Circadian clocks operative in pancreatic islets participate in the regulation of insulin secretion in humans and, if compromised, in the development of type 2 diabetes (T2D) in rodents. Here we demonstrate that human islet ?- and ?-cells that bear attenuated clocks exhibit strongly disrupted insulin and glucagon granule docking and exocytosis. To examine whether compromised clocks play a role in the pathogenesis of T2D in humans, we quantified parameters of molecular clocks operative in human T2D islets at population, single islet, and single islet cell levels. Strikingly, our experiments reveal that islets from T2D patients contain clocks with diminished circadian amplitudes and reduced in vitro synchronization capacity compared to their nondiabetic counterparts. Moreover, our data suggest that islet clocks orchestrate temporal profiles of insulin and glucagon secretion in a physiological context. This regulation was disrupted in T2D subjects, implying a role for the islet cell-autonomous clocks in T2D progression. Finally, Nobiletin, an agonist of the core-clock proteins ROR?/?, boosted both circadian amplitude of T2D islet clocks and insulin secretion by these islets. Our study emphasizes a link between the circadian clockwork and T2D and proposes that clock modulators hold promise as putative therapeutic agents for this frequent disorder.
Authors
Volodymyr Petrenko, Nikhil R. Gandasi, Daniel Sage, Anders Tengholm, Sebastian Barg, and Charna Dibner.
Acknowledgments
The authors thank Jacques Philippe, Ueli Schibler, and Claes Wollheim (University of Geneva) for constructive discussions; Marie-Claude Brulhart-Meynet (University Hospital of Geneva) for skillful technical assistance; Domenico Bosco and Thierry Berney (Islet Transplantation Center of Geneva University Hospital), Eduard Montanya Mias and Montserrat Nacher Garcia (Hospital Universitari de Bellvitge, Barcelona) for providing human islets; Etienne Lefai (Institut National de la Recherche Agronomique Auvergne Rhône-Alpes) for adenovirus amplification; Andre Liani and George Severi (University of Geneva) for assistance with perifusion experiments; and Christoph Bauer and Jerome Bosset (University of Geneva) for support with bioimaging experiments. Human islets from the Islet Transplantation Center of Geneva University Hospital were provided through Juvenile Diabetes Research Foundation Award 31-2008-416 (European Consortium for islet transplantation (ECIT) islet for Basic Research program, Thierry Berney). This work was funded by Swiss National Science Foundation Grants 31003A_166700/1, 310030_184708/1, the Vontobel Foundation, the Novartis Consumer Health Foundation, Bo and Kerstin Hjelt Foundation for diabetes type 2, Swiss Life Foundation, and the Olga Mayenfisch Foundation (C.D.); Swedish Research Council 2017-00956, 2018-02871 (to S.B. and A.T.); and Family Ernfors Foundation, European Foundation for the Study of Diabetes, Novo Nordisk Foundation, Diabetes Wellness Network Sweden, Swedish Diabetes Foundation, Exodiab network, Hjärnfonden (S.B.). N.R.G. was supported by the European Foundation for the Study of Diabetes–Rising Star Program and Novo Nordisk Foundation–Young Investigator Program.
Return to top of page.
| |
|
Feb 3 2020 Fetal Timeline Maternal Timeline News
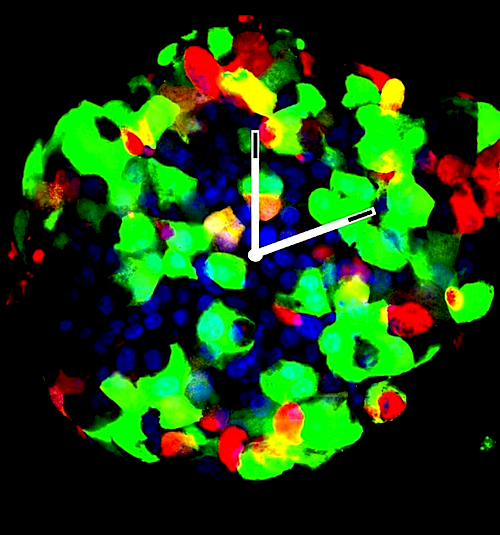
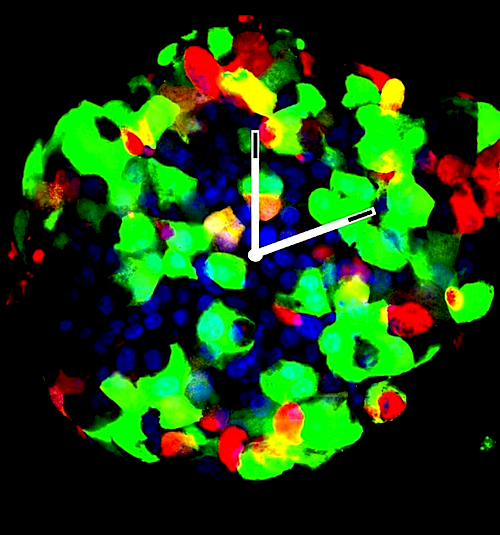 A Langerhans Islet with insulin-producing cells (GREEN), and glucagon-producing cells (RED). Cell nuclei in BLUE. CREDIT © UNIGE/ Dibner Lab.
|