|
|
Developmental Biology - Enzyme Replacement Therapy
Stem Cells Given to Fetus Treat Metabolic Disorders
Fetal stem cell/enzyme therapy may alleviate some congenital diseases that often result in pregnancy loss...
According to a new study in the journal Science Translational Medicine University of California San Francisco (UCSF) researchers, have devised a way to introduce stem cells into the fetal brain during prenatal development with the goal of making up for cells that cannot produce an essential protein causing dysfunction of multiple organs, including the brain — and may also be undiagnosed cause of fetal deaths.
Each year, about 24,000 women in the US lose a pregnancy. One of the major contributors to this problem is a group of congenital diseases that can cause a condition called hydrops, in which fluid accumulates in the fetus, often fatally.
Tippi MacKenzie PhD, Co-Director, UCSF Center for Maternal-Fetal Precision Medicine, San Francisco, California, USA.
"This group of vulnerable patients has been relatively ignored in the fetal surgery world," said UCSF's Tippi MacKenzie MD, senior author of the new study who has worked for a decade developing novel therapies for heritable diseases that can be treated before birth. "We know these patients could potentially benefit from a number of medical therapies. So this is our first foray into treating one of those diseases."
The new study was aimed at exploring treatments for MPS7, also known as Sly syndrome, a disorder caused by a mutation in a single gene. In this disease the body lacks an enzyme to correctly process large chains of sugar molecules needed for correct cell function. Sly syndrome is part of a family of related metabolic disorders that can potentially be treated before birth using similar approaches.
The incidence of MPS7 is difficult to determine, as it is believed many fetuses with the disorder die before birth. Those that survive are treated by regular injections of the missing B-glucuronidase enzyme. While these injections provide some benefit, the enzyme cannot enter the brain through the bloodstream following birth. In some related metabolic diseases, clinicians need to infuse the enzyme directly into the brain to treat the resulting neurological effects.
As the 'blood-brain barrier' protecting the brain from potential damage by blood born substances is not fully developed before a baby is born, MacKenzie believes the enzyme can be successfully introduced into the fetus before birth.
Another problem with repeated enzyme infusions for metabolic disorders is that patients can develop an immune reaction. Their bodies view the enzyme as "foreign." Infusing the protein before birth could prevent this, as fetal immune systems tend to view all new proteins as "friendly" and not reject them.
MacKenzie is among the first to attempt enzyme replacement of any sort in the fetal stage. Led by co-first author Russell Witt MD, these experiments proved successful. Researchers discovered that in utero treatment with the B-glucuronidase enzyme dramatically improved survival of mice to birth. Researchers continued to give the enzyme after birth, ultimately resulting in immune tolerance of the enzyme and improvements in multiple organs, including the brain and liver.
Moreover, in comprehensive testing of these mice in collaboration with the UCSF lab of Saul Villeda PhD, researchers observed significantly improved strength in the grip of MPS7 mice, which is generally weak. In some cases that grip strength approached normal.
All told, the research team found in utero enzyme replacement conferred three major improvements. Explains MacKenzie:
(1) The enzyme will cross the blood/brain barrier
(2) Immune tolerance high with early introduction
(3) Treatment helps sustain fetus through birth.
These combined advantages overcome the main limitations to the current approach of delivering enzyme treatment after birth - but not all. Even if treatment is successfully delivered in the womb, challenges would still exist as the enzyme only lasts about two weeks in the body. Thus, patients would still require regular injections following birth after the blood-brain barrier fully develops.
Ultimately, explains MacKenzie, the answer may lie in giving a fetus stem cells in both brain and body.
To explore this possibility, MacKenzie worked with research fellow and surgery resident Quoc-Hung Nguyen MD, to transplant blood-forming stem cells from normal mice into fetal mice carrying a genetic mutation causing MPS7. Researchers wanted to see whether stem cells could reach the brain, and whether they change into microglia immune cells that originate from blood-forming stem cells.
In normal fetal development, mature microglia produce and store the B-glucuronidase enzyme, and regulate the immune environment of the brain.
Others have tried transplanting these stem cells, but usually after birth, says Nguyen. It has been challenging to obtain fully functioning microglia. "We wanted to test this transplant before birth, using the environment of the fetal brain where, in a normal fetus, the stem cells are migrating into the brain to become microglia," he said. "One of our big findings is that these cells truly do become microglia, so there's a huge advantage to transplanting them before birth."
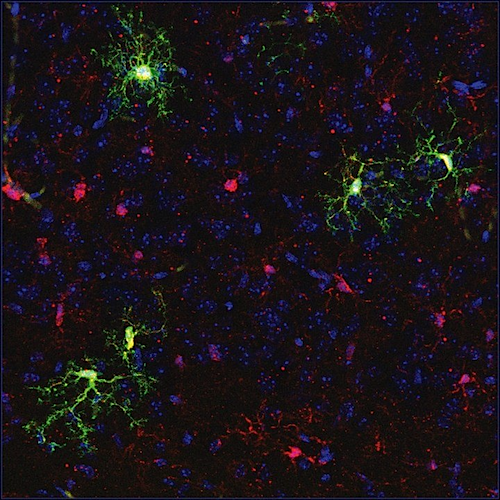
Nguyen tagged the transplanted cells with a fluorescent marker so he could easily identify them and verify that they had successfully crossed the blood-brain barrier and migrated into the brain. To confirm that the transplanted cells were acting as functional microglia, Nyugen sequenced the RNA that the cells were producing and saw that it matched the proper signature of protein production by microglia.
He also confirmed that the stem cells had also made their way to the liver, kidney, and other organs, where they became the appropriate cell type needed to produce needed enzymes to those organs.
Researchers saw once these stem cells engrafted in the brain and body and differentiated — they delivered the enzyme to nearby cells and restored their function, a process called cross-correction. These transplanted cells fended off liver disease and other complications associated with MPS7 for the lifespan of the animals.
"We found that even if you have only one or two percent healthy cells circulating, you can drastically improve, for example, liver disease. One good cell can, in effect, correct multiple other cells," explains MacKenzie.
An advantage of this treatment is that it could be performed using fetal blood transfusions in hospitals around the world. "That means that if we do perform fetal therapy for these diseases in humans, the treatments could someday be offered at multiple centers around the world, and the family doesn't have to travel a long distance to get the care they need," adds MacKenzie. There are a large number of other heritable metabolic disorders that arise from similar faulty single genes. Nyugen and MacKenzie agree that their approach may be a useful one for these conditions as well.
"These exciting findings are just the tip of the iceberg," says Nyugen. "They open up a whole new approach to treating a range of diseases. At the same time, there's also a lot of work to do to optimize the treatment for humans."
MacKenzie is now applying to the U.S. Food and Drug Administration to launch a clinical trial of enzyme replacement therapy that will ultimately enroll 10 patients with MPS7 and related metabolic disorders. She already has a similar trial underway, transplanting mothers' stem cells into developing fetuses to treat a blood disorder called alpha thalassemia. With the proposed trial of enzyme replacement therapy, she hopes to expand the scope of fetal molecular therapies to treat metabolic disorders as well as blood disorders in humans.
MacKenzie points out that while fetal molecular therapies are not yet common, the environment and resources at UCSF allow her team to broaden the field, even as it develops.
"With this work, we're pushing the frontiers of fetal surgery into newer, less invasive therapies. At the same time, colleagues at UCSF are performing genetic sequencing of fetuses with hydrops, so that one day we can identify and treat these genetic conditions before birth. It's exactly this sort of clinical and research environment that can accelerate moving a therapy like this one into humans."
Tippi MacKenzie PhD.
Abstract
Mucopolysaccharidosis type VII (MPS7) is a lysosomal storage disorder (LSD) resulting from mutations in the B-glucuronidase gene, leading to multiorgan dysfunction and fetal demise. While postnatal enzyme replacement therapy (ERT) and hematopoietic stem cell transplantation have resulted in some phenotypic improvements, prenatal treatment might take advantage of a unique developmental window to penetrate the blood-brain barrier or induce tolerance to the missing protein, addressing two important shortcomings of postnatal therapy for multiple LSDs. We performed in utero ERT (IUERT) at E14.5 in MPS7 mice and improved survival of affected mice to birth. IUERT penetrated brain microglia, whereas postnatal administration did not, and neurological testing (after IUERT plus postnatal administration) showed decreased microglial inflammation and improved grip strength in treated mice. IUERT prevented antienzyme antibody development even after multiple repeated postnatal challenges. To test a more durable treatment strategy, we performed in utero hematopoietic stem cell transplantation (IUHCT) using congenic CX3C chemokine receptor 1–green fluorescent protein (CX3CR1-GFP) mice as donors, such that donor-derived microglia are identified by GFP expression. In wild-type recipients, hematopoietic chimerism resulted in microglial engraftment throughout the brain without irradiation or conditioning; the transcriptomes of donor and host microglia were similar. IUHCT in MPS7 mice enabled cross-correction of liver Kupffer cells and improved phenotype in multiple tissues. Engrafted microglia were seen in chimeric mice, with decreased inflammation near donor microglia. These results suggest that fetal therapy with IUERT and/or IUHCT could overcome the shortcomings of current treatment strategies to improve phenotype in MPS7 and other LSDs.
Authors
Quoc-Hung Nguyen, Russell G. Witt, Bowen Wang, Carlo Eikani, Jeremy Shea, Lucas K. Smith, Gabrielle Boyle, Jaclyn Cadaoas, Renan Sper, John D. MacKenzie, Saul Villeda and Tippi C. MacKenzie.
Acknowledgements
Funding: This study was supported by a grant from Ultragenyx to Tippi MacKenzie, funds from the UCSF Center for Maternal-Fetal Precision Medicine, a CIRM New Faculty grant to Tippi MacKenzie (RN3-06532), and NIH grant support (5T32HD007263-35) to Nguyen.
Disclosures: Co-authors Boyle and Cadaoas are employees of Ultragenyx.
About UCSF: The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF's primary academic medical center, includes top-ranked specialty hospitals and other clinical programs, and has affiliations throughout the Bay Area. Learn more at https://www.ucsf.edu, or see our Fact Sheet.
About ISGlobal
The Barcelona Institute for Global Health, ISGlobal, is the fruit of an innovative alliance between "la Caixa" and academic and government institutions to contribute to the efforts undertaken by the international community to address the challenges in global health. ISGlobal is a consolidated hub of excellence in research that has grown out of work first started in the world of health care by the Hospital Clínic and the Parc de Salut MAR and in the academic sphere by the University of Barcelona and Pompeu Fabra University. The pivotal mechanism of its work model is the transfer of knowledge generated by scientific research to practice, a task undertaken by the institute's Education and Policy and Global Development departments. ISGlobal has been named a Severo Ochoa Centre of Excellence and is a member of the CERCA programme of the Generalitat de Catalunya.
Return to top of page.
| |
|
Feb 28 2020 Fetal Timeline Maternal Timeline News
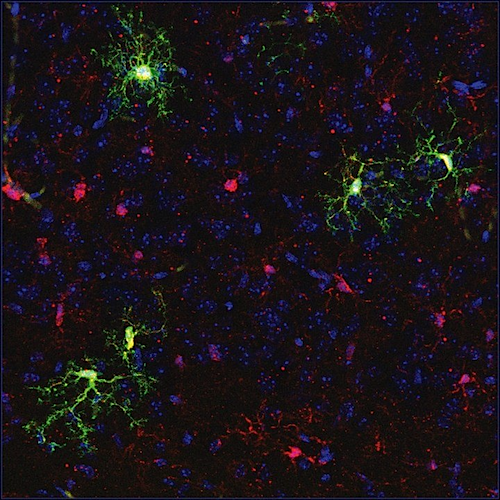 Stem cells (GREEN) transplanted into fetal mouse in utero, graft into fetal mouse brain tissue. CREDIT Q-H Nguyen/MacKenzie lab
|