|
|
Developmental Biology - COVID-19
COVID-19 Triggers Deadly Blood Clots
Understanding underlying causes of these clots could possibly lead to treatments to prevent them happening...
Changes in blood platelets triggered by COVID-19 could contribute to the onset of heart attacks, strokes, and other serious complications, in some patients who have the disease, according to University of Utah Health scientists.
Researchers found that inflammatory proteins produced during infection significantly alter the function of platelets, making them "hyperactive" and more prone to form dangerous and potentially deadly blood clots.
Better understanding the underlying causes of these changes could possibly lead to treatments preventing them from happening in COVID-19 patients. The report appears in BLOOD, an American Society of Hematology journal.
"Our finding adds an important piece to the jigsaw puzzle that we call COVID-19," says Robert A. Campbell PhD, senior author of the study and an assistant professor in the Department of Internal Medicine. "We found that inflammation and systemic changes, due to the infection, are influencing how platelets function, leading them to aggregate faster, which could explain why we are seeing increased numbers of blood clots in COVID patients."
Emerging evidence suggests COVID-19 is associated with an increased risk of blood clotting, which can lead to cardiovascular problems and organ failure in some patients, particularly among those with underlying medical problems such as diabetes, obesity, or high blood pressure.
To find out what might be going on, the researchers studied 41 COVID-19 patients hospitalized at University of Utah Hospital in Salt Lake City. Seventeen of these patients were in the ICU, including nine who were on ventilators. They compared blood from these patients with samples taken from healthy individuals who were matched for age and sex.
Using differential gene analysis, the researchers found that SARS-CoV-2, the virus that causes COVID-19, appears to trigger genetic changes in platelets. In laboratory studies, they studied platelet aggregation, an important component of blood clot formation, and observed COVID-19 platelets aggregated more readily.
They also noted that these changes significantly altered how platelets interacted with the immune system, likely contributing to inflammation of the respiratory tract that may, in turn, result in more severe lung injury.
Surprisingly, Campbell and his colleagues didn't detect evidence of the virus in the vast majority of platelets, suggesting that it could be promoting the genetic changes within these cells indirectly.
One possible mechanism is inflammation, according to Bhanu Kanth Manne PhD, one of the study's lead authors and a research associate with the University of Utah Molecular Medicine Program (U2M2).
In theory, inflammation caused by COVID-19 could affect megakaryocytes, the cells that produce platelets. As a result, critical genetic alterations are passed down from megakaryocytes to the platelets, which, in turn, make them hyperactive.
In test tube studies, the researchers found that pre-treating platelets from SARS-CoV-2 infected patients with aspirin did prevent this hyperactivity. These findings suggest aspirin may improve outcomes; however, this will need further study in clinical trials. For now, Campbell warns against using aspirin to treat COVID-19 unless recommended by your physician.
In the meantime, the researchers are beginning to look for other possible treatments.
"There are genetic processes that we can target that would prevent platelets from being changed. If we can figure out how COVID-19 is interacting with megakaryocytes or platelets, then we might be able to block that interaction and reduce someone's risk of developing a blood clot."
Robert A. Campbell PhD, Assistant Professor, Department of Internal Medicine, George and Dolores Eccles Institute of Human Genetics, and senior author; University of Utah School of Medicine, Salt Lake City, Utah, USA.
Abstract
Key Points
Neutrophil Extracellular Traps (NETs) contribute to microthrombi through platelet-neutrophil interactions in COVID-19 ARDS
Neonatal NET-Inhibitory Factor (nNIF) blocks NETs induced by COVID-19 plasma and represents a potential therapeutic intervention in COVID-19
COVID-19 affects millions of patients worldwide with clinical presentation ranging from isolated thrombosis to acute respiratory distress syndrome (ARDS) requiring ventilator support. Neutrophil extracellular traps (NETs) originate from decondensed chromatin released to immobilize pathogens and can trigger immunothrombosis. We studied the connection between NETs and COVID-19 severity and progression. We conducted a prospective cohort study of COVID-19 patients (n=33) with age- and sex-matched controls (n=17). We measured plasma myeloperoxidase (MPO)-DNA complexes (NETs), Platelet Factor 4, RANTES, and selected cytokines. Three COVID-19 lung autopsies were examined for NETs and platelet involvement. We assessed NET formation ex vivo in COVID-19 neutrophils and in healthy neutrophils incubated with COVID-19 plasma. We also tested the ability of neonatal NET-Inhibitory Factor (nNIF) to block NET formation induced by COVID-19 plasma. Plasma MPO-DNA complexes increased in COVID-19 with intubation (P<0.0001) and death as outcome (P<0.0005). Illness severity correlated directly with plasma MPO-DNA complexes (P=0.0360), while PaO2/FiO2 correlated inversely(P=0.0340). Soluble and cellular factors triggering NETs were significantly increased in COVID-19 and pulmonary autopsies confirmed NET-containing microthrombi with neutrophil-platelet infiltration. Finally, COVID-19 neutrophils ex vivo displayed excessive NETs at baseline and COVID-19 plasma triggered NET formation which was blocked by nNIF. Thus, NETs triggering immunothrombosis may, in part, explain the prothrombotic clinical presentations in COVID-19 and NETs may represent targets for therapeutic intervention.
Authors
Elizabeth A Middleton, Xue-Yan He, Frederik Denorme, Robert A. Campbell, David Ng, Steven P. Salvatore, Maria Mostyka, Amelia Baxter-Stoltzfus, Alain C. Borczuk, Massimo Loda, Mark J. Cody, Bhanu Kanth Manne, Irina Portier, Estelle Harris, Aaron C. Petrey, Ellen J. Beswick, Aleah F. Caulin, Anthony Iovino, Lisa M. Abegglen, Andrew S. Weyrich, Matthew T. Rondina, Mikala Egeblad, Joshua David Schiffman and Christian Con Yost.
Acknowledgements
This study was funded by the National Institutes of Health, the University of Utah Health 3i Initiative, and the American Heart Foundation.
Return to top of page.
|
|
Jul 2 2020 Fetal Timeline Maternal Timeline News
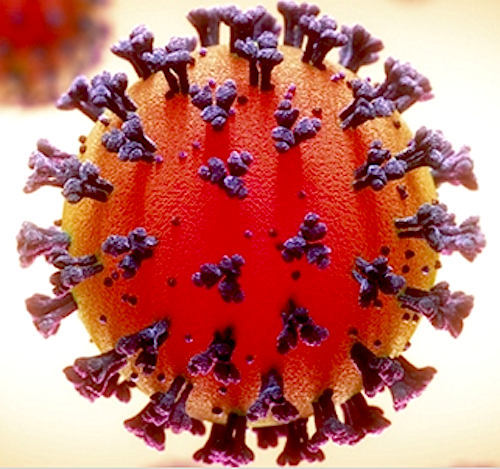 A computer simulated model of COVID19. CREDIT Public Domain
|
|

