|
|
Developmental Biology - COVID19
Lung Physiology and Immune Function in Children
Lung and immune differences between children and adults could be protecting some children from severe COVID-19...
Differences in lung physiology and immune function in children could be why they are more often spared from severe illness associated with COVID-19 than adults. This hypothesis was the basis of a grant from the National Heart, Lung, and Blood Institute awarded to Krithika Lingappan MD, Assistant Professor, Pediatrics and Newborns, Baylor College of Medicine
Houston, Texas, USA.
According to Dr. Lingappan, physicians along with scientists need to analyse these disparities between symptoms in age groups.
The paper was recently published in American Journal of Physiology-Lung Cellular and Molecular Physiology.
Only about 1.7% of the first 149,082 cases in the USA have been infants, children, and adolescents younger than 18 years old — while children under 18 make up 22% of our entire population. Only three pediatric deaths were identified by the Centers for Disease Control and Prevention (CDC) as of April 2020.
"These profoundly decreased rates of symptomatic infection, hospitalization, and death are well beyond statistical significance, require further examination, and may hold the key to identifying therapeutic agents," Lingappan writes.
Angiotensin-converting enzyme 2, called ACE2, allow SARS-CoV-2 — the novel coronavirus that causes COVID-19 — to enter our body's cells.
Children have less ACE2 in their lungs than adults.
"Angiotensin-converting enzymes are important for viral entry. There seem to be less of them in children — but they increase with age," explains Matthew Harting MD MS and assistant professor in the Department of Pediatric Surgery at McGovern Medical School, UTHealth.
In addition to fewer ACE2 receptors, the authors note the immune system in children responds to viruses differently than that of adults, leaving less opportunity for severe illness in pediatric patients. There are several different mechanisms behind the differences, including the retention of T-cells in children, which are able to fight off or limit inflammation.
"T-cells have a viral response and also an immune modulator response. In severe cases of adult COVID-19 patients, we've seen those T-cells are reduced, so the ability to fight the virus is also reduced. In kids, those T-cells seem to be maintained, so they are still able to prevent the virus."
[CDC Laboratory-Confirmed Influenza Hospitalizations]
Harry Karmouty-Quintana PhD, Assistant Professor, Department of Biochemistry and Molecular Biology at McGovern Medical School, and a co-author on the paper.
Lung tissue in children naturally has a higher concentration of regulator T-cells. Patients with higher levels of T-cells also have higher levels of Interleukin 10 (IL-10), also known as human cytokine synthesis inhibitory factor, an anti-inflammatory cytokine.
"IL-10 inhibits the inflammation of other components like IL-6 that are detrimental. Adults tend to experience hyperinflammatory state, where kids do not," addsKarmouty-Quintana. "In preclinical studies in mice, IL-10 has also shown to decrease with age."
The paper's findings were made possible through collaboration in a multidisciplinary group made up of pediatric and adult physicians and scientists in pediatric surgery, adult critical care, neonatology, and molecular biology.
"We physicians have been challenged with how to treat COVID-19 and we're learning in real time. I knew to figure out the best way to treat adults, we needed to team together to get to the bottom of why children were being spared severe illness related to the virus."
Bindu Akkanti MD, Associate Professor, Critical Care Medicine, McGovern Medical School; Attending Physician, Critical Care, Memorial Hermann-Texas Medical Center, study first author.
"Moving forward, physicians and scientists need multi-disciplinary collaboration to continue learning - another step in the right direction to attack this virus."
Krithika Lingappan MD MBBS. Assistant Professor, Pediatrics, Baylor College of Medicine; Neonatologists, Texas Children's Hospital.
As a result of this collaboration, a new study has begun of patients in different stages of COVID-19. The goal being to better understand disparities in progression between children and adults.
Abstract
The rapid emergence and subsequent global dissemination of SARS-CoV-2 disease (COVID-19) has resulted in over 4 million cases worldwide. The disease has a marked predilection for adults, and children are relatively spared. Understanding the age-based differences in pathophysiological pathways and processes relevant to the onset and progression of disease both in the clinical course and in experimental disease models may hold the key to the identification of therapeutic targets. The differences in the clinical course are highlighted by the lack of progression of the SARS-CoV-2 infection beyond mild symptoms in a majority of children, whereas in adults the disease progresses to acute lung injury and an acute respiratory distress syndrome (ARDS)-like phenotype with high mortality. The pathophysiological mechanisms leading to decreased lung injury in children may involve the decreased expression of the mediators necessary for viral entry into the respiratory epithelium and differences in the immune system responses in children. Specifically, decreased expression of proteins, including angiotensin-converting enzyme 2 (ACE2) and Transmembrane Serine Protease 2 (TMPRSS2) in the airway epithelium in children may prevent viral entry. The immune system differences may include a relative preponderance of CD4+ T cells, decreased neutrophil infiltration, decreased production of proinflammatory cytokines, and increased production of immunomodulatory cytokines in children compared with adults. Notably, the developing lung in children may have a greater capacity to recover and repair after viral infection. Understanding the relative contributions of the above processes to the protective phenotype in the developing lung can guide the trial of the appropriate therapies in adults.
Authors
Krithika Lingappan MD, Harry Karmouty-Quintana PhD, Jonathan Davies MD, Bindu Akkanti MD CMQ FCCP, and Matthew T. Harting, MD, MS.
Acknowledgements
This work was supported in part by National Heart, Lung, and Blood Institute Grants R01HL144775 and R01HL146395 to Krithika Lingappan MD.
Disclosures
No conflicts of interest, financial or otherwise, are declared by the authors.
Return to top of page.
|
|
Jul 9 2020 Fetal Timeline Maternal Timeline News
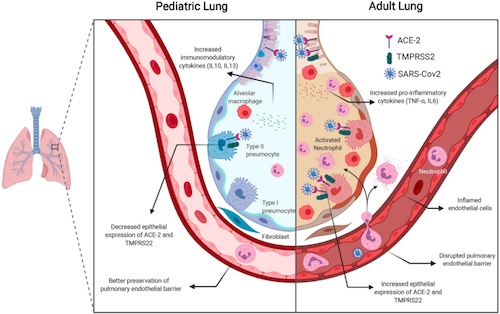 Comparison of physiology of a PEDIATRIC and ADULT lung. CREDIT Krithika Lingappan, Matthew Harting and Bindu Akkanti.
|
|

