|
|
Developmental Biology - COVID-19/Placenta
What Prevents COVID-19 Entering Baby via Placenta?
Protection of the placenta offers opportunities for future study of COVID-19 transmission prevention...
Researchers from Boston Medical Center, Maxwell Finland Laboratory for Infectious Disease, have identified properties in placental tissue that may give it an important edge in preventing transmission of COVID-19 from a virally active mother to her fetus.
This study demonstrates that COVID-19 universally invades the placenta with and without evidence of fetal infection, highlighting how it may offer protection against COVID-19. Current data indicates a less than five percent COVID-19 transmission rate in newborns from their infected mothers.
Published in Placenta, these results underscore the importance of using placenta tissue in COVID-19 research aimed at developing novel ways to diagnose, treat and prevent COVID-19 viral transmission.
Researchers examined placental tissue as it shares developmental and physiologic similarities with human lung and immune responses, including those of the small and large intestines. The placenta may therefore be a key tissue source for ongoing COVID-19 research. Placental tissue also contains a unique expression pattern of COVID-19 receptors different from other organ systems, which would be useful in defining its reaction to COVID-19 treatments.
"This study provides evidence for ongoing research of COVID-19 infection at the maternal-fetal interface as a means to better understand viral transmission and infection to other human tissues. Previous research has shown the placenta protects a fetus from various types of infection. Exploring the particular ways it protects the fetus from COVID-19 transmission, may help identify new targets of COVID-19 prevention and treatment."
Elisha Wachman MD, Neonatologist, Boston Medical Center; Associate Professor, Department of Pediatrics, Boston University School of Medicine; and principal investigator of this study.
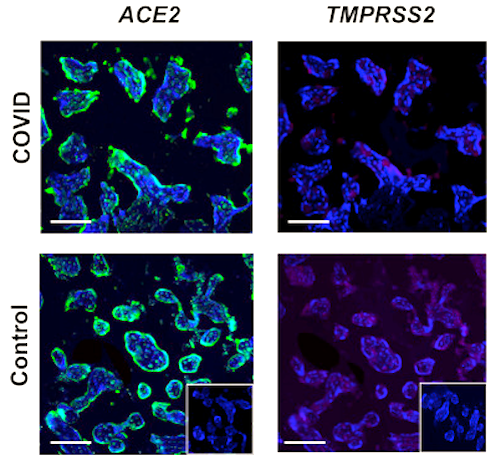
Throughout April and May 2020, samples from 15 COVID-19 positive maternal-fetal dyads were collected for this study. Five cases with evidence of fetal transmission. The placental tissue of positive cases were analyzed and compared with the ten negative COVID-19 controls. Researchers found the COVID-19 virus present in placental tissues with and without evidence of fetal infection. They also found the placenta contains a unique pattern of cell surface proteins — TMPRSS2 and ACE2 — important for COVID-19 viral entry, unique from other tissue types. The demographics of mother-baby dyads also reflected no significant differences, supporting fetal transmission does not discriminate.
"As a readily available tissue for research, the placenta can be a valuable source of scientific study for a variety of human diseases in pregnancy and beyond."
Elisha Wachman MD
Abstract Highlights
• SARS-CoV2 glycoprotein in the placenta does not vary with fetal transmission.
• SARS-CoV-2 viral entry protein ACE2 is highly expressed in the villous placenta.
• SARSS-CoV-2 viral entry protein TMPRSS2 has low expression in the villous placenta.
Abstract
Introduction
While the COVID-19 pandemic continues to have a significant global health impact, rates of maternal to infant vertical transmission remain low (<5%). Parenchymal changes of placentas from COVID-19 infected mothers have been reported by several groups, but the localization and relative abundance of SARS-CoV-2 viral proteins and cellular entry machinery has not been fully characterized within larger placental tissue cohorts.
Methods
An extended placental tissue cohort including samples from 15 COVID-19 positive maternal-fetal dyads (with n = 5 cases with evidence of fetal transmission) in comparison with 10 contemporary COVID-19 negative controls. Using comparative immunofluorescence, we examined the localization and relative tissue abundance of SARS-CoV2 spike glycoprotein (CoV2 SP) along with the co-localization of two SARS-CoV2 viral entry proteins angiotensin-converting enzyme 2 (ACE2) and transmembrane serine protease 2 (TMPRSS2).
Results/conclusions
CoV2 SP was present within the villous placenta in COVID-19 positive pregnancies with and without evidence of fetal transmission. We further identified the predominance of ACE2 expression in comparison with TMPRSS2. Importantly, both CoV2 SP and ACE2 expression consistently localized primarily within the outer syncytiotrophoblast layer placental villi, a key physiologic interface between mother and fetus. Overall this study provides an important basis for the ongoing evaluation of SARS-CoV-2 physiology in pregnancy and highlights the importance of the placenta as a key source of primary human tissue for ongoing diagnostic and therapeutic research efforts to reduce the global burden of COVID-19.
Authors
Elizabeth Taglauera, Yoel Benarroch, Kevin Rop, Elizabeth Barnett, Vishakha Sabharwal, Christina Yarrington and Elisha M. Wachman.
Acknowledgements
The authors would like to thank the Department of Pathology at Boston Medical Center for their support and collaboration, particularly Elizabeth Duffy, Charline Mack, and Cheryl Spencer. We would also like to thank the Boston University Medical Campus Alumni Library, the Boston University School of Medicine Cellular Imaging Core and everyone in the Finland Laboratory for Pediatric Infectious Disease at Boston Medical Center, particularly lab manager Yazdan Dasthagrasaheb for all of his support, and laboratory technician Loc Truong. This work was funded by the Boston University Clinical and Translational Science Institute COVID-19 Pilot Grant Program (UL1TR001430), NIH T32 1T32HD098061-01 (EST) and the Boston University School of Medicine Medical Student Summer Research Program.
Funding for this study was provided by the Boston University Clinical and Translational Science Institute COVID-19 Pilot Grant Program (UL1TR001430), NIH T32 1T32HD098061-01 (EST) and the Boston University School of Medicine Medical Student Summer Research Program.
About Boston Medical Center
Boston Medical Center is a private, not-for-profit, 514-bed, academic medical center that is the primary teaching affiliate of Boston University School of Medicine. It is the largest and busiest provider of trauma and emergency services in New England. Boston Medical Center offers specialized care for complex health problems and is a leading research institution, receiving more than $97 million in sponsored research funding in fiscal year 2018. It is the 15th largest funding recipient in the U.S. from the National Institutes of Health among independent hospitals. In 1997, BMC founded Boston Medical Center Health Plan, Inc., now one of the top ranked Medicaid MCOs in the country, as a non-profit managed care organization. Boston Medical Center and Boston University School of Medicine are partners in Boston HealthNet - 14 community health centers focused on providing exceptional health care to residents of Boston. For more information, please visit http://www.bmc.org.
Return to top of page.
| |
|
Sep 8 2020 Fetal Timeline Maternal Timeline News
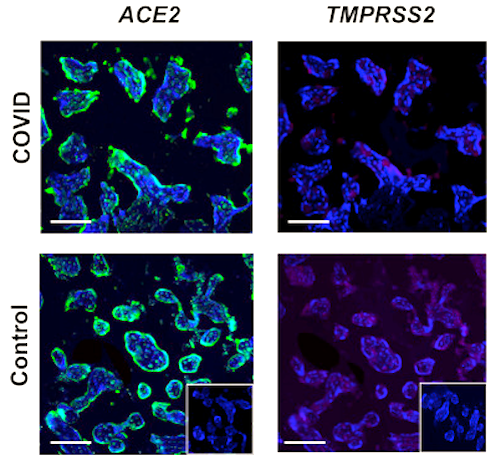 Placental Analysis via Fluorescence TOP: COVID infected placenta BOTTOM: Uninfected Control Placenta.CREDIT The Authors.
|