|
|
Developmental Biology - Newborn Brain Hemorrhage
Newborn Asymptomatic Brain Hemorrhage
Asymptomatic brain bleeds in newborns show up as normal brain development by age 2...
A new study finds neurodevelopmental scores and gray matter volume of two years old, is no different between those born with MRI-confirmed asymptomatic subdural brain hemorrhages and babies born with no in uterine history of brain bleeds.
In 2007, UNC researchers published unexpected and surprising results from a study based on magnetic resonance imaging (MRI) of newborn brains. Twenty-six percent of the newborns in the study were found to have asymptomatic subdural hemorrhages, or bleeding in and around the brain.
It was an unexpected finding as subdural hemorrhage had been considered unusual in full-term newborns. But, these 2007 findings suggest that small, asymptomatic brain bleeds might be a fairly common consequence of a normal vaginal delivery.
Now 13 years later, John H. Gilmore MD, professor, vice chair of research, UNC Department of Psychiatry and senior author of the 2007 study, along with J. Keith Smith, MD, PhD, vice chair, UNC Department of Radiology. have published a follow-up study in the journal Radiology, the journal which also published the 2007 study.
"We were one of the first groups to systematically scan the brains of newborns and were very surprised to discover that small subdural bleeds are very common. As the bleeds were so common, we believed they did not have a significant impact on brain development, but had no hard data to know for sure.
This follow-up study is reassuring and demonstrates that children with these minor perinatal bleeds have normal cognitive development at two years of age."
John H. Gilmore MD, senior author of the new study and director of the UNC Center of Excellence in Community Mental Health.
The new article is based on data collected from 311 infants between 2003 and 2016. Outcomes of neurodevelopment were evaluated at two years of age using the Mullen Scales of Early Learning (MSEL). All infants had MRI brain scans and were evaluated for subdural hemorrhage as neonates, also at ages one and two years.
In comparing children with a history of subdural hemorrhage to those without, study authors found no differences between the two groups in either MSEL scores or in total gray matter volumes. Also, at age two there was no evidence of rebleeding in the children who had subdural hemorrhage as neonates.
"There are two really important findings of this work. These small bleeds, which are very common, do not seem to harm brain development, and they also go away and don't predispose to later bleeding or other abnormalities."
J. Keith Smith MD PhD, professor, interim chair, department of radiology; University of North Carolina Chapel Hill, School of Medicine, North Carolina, USA.
Abstract Summary
Neurodevelopmental outcomes and gray matter volumes at age 2 years did not differ between asymptomatic neonates with subdural hemorrhage and those with normal neonatal MRI findings.
Background
Subdural hemorrhage (SDH) is thought to have a benign course in asymptomatic neonates. However, effects on neurodevelopmental outcomes have not been established.
Purpose
To evaluate neurodevelopmental outcomes, gray matter volumes, and MRI findings in asymptomatic neonates with SDH compared with control neonates.
Materials and Methods
This retrospective analysis was conducted between 2003 and 2016 and was based on data from the University of North Carolina Early Brain Development Study. Neurodevelopmental outcomes were evaluated at 2 years of age by using the Mullen Scales of Early Learning (MSEL). All infants were imaged with 3.0-T MRI machines and were evaluated for SDH at baseline (neonates) and at ages 1 and 2 years. Volumetric MRI for brain segmentation was performed at ages 1 and 2 years. A secondary analysis was performed in neonates matched 1:1 with control neonates. Differences in categorical variables were measured by using the Fisher exact test, and the t test was used for continuous variables.
Results
A total of 311 neonates (mean gestational age ± standard deviation, 39.3 weeks ± 1.5), including 57 with SDH (mean gestational age, 39.5 weeks ± 1.2), were evaluated. The subgroup included 55 neonates with SDH (mean gestational age, 39.6 weeks ± 1.2) and 55 matched control neonates (mean gestational age, 39.7 weeks ± 1.2). Fifty-five of 57 neonates with SDH (97%; 95% CI: 92, 100) were delivered vaginally compared with 157 of 254 control neonates (62%, 95% CI: 56, 68; P < .001). Otherwise, there were no differences in perinatal, maternal, or obstetric parameters. There were no differences in composite MSEL scores (115 ± 15 and 109 ± 16 at 2 years, respectively; P = .05) or gray matter volumes between the neonatal SDH group and control neonates (730 cm3 ± 85 and 742 cm3 ± 76 at 2 years, respectively; P = .70). There was no evidence of rebleeding at follow-up MRI.
Conclusion
Neurodevelopmental scores and gray matter volumes at age 2 years did not differ between asymptomatic neonates with subdural hemorrhage and control neonates.
Authors
Co-authors of the study are Carlos Zamora, MD, PhD; Cassandra Sams, MD; Emil A. Cornea, PhD; and Zhenhua Yuan, PhD.
Acknowledgements
The study was supported by grants from the National Institutes of Health (MH064065, MH070890, HD053000).
Return to top of page.
|
|
Nov 17 2020 Fetal Timeline Maternal Timeline News
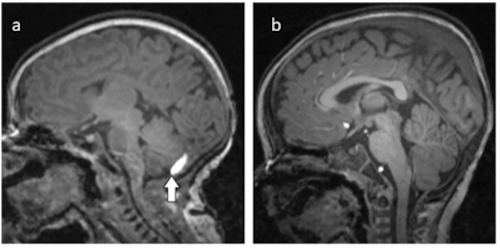
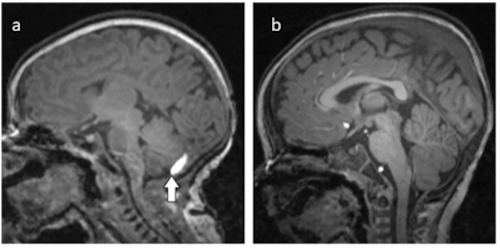 (A) Fifteen day old neonate with brain bleed at arrow. (B) Twelve months later with Normal MRI. CREDIT Zamora C, et al.
| |